MyThy Huynh is a nurse who lives in Southwest Detroit with her boyfriend Matt. She is also known to food lovers in Detroit and beyond as @mightyinthemitten on Instagram and through her pop-ups and cooking classes around town. We asked her to share her experience on the frontlines during the COVID-19 pandemic. Here is her story.
Is it real?
March 2
I think I got the ‘Rona on this day.
I’m sick and believe my ulcer is acting up as I wake up with abdominal pain. This time it’s accompanied with nausea and vomiting. When my ulcer acts up (once or twice a year), I normally am nauseous and it’s usually resolved by lying in a fetal position for an hour or so. I don’t vomit but this time I do after water, saltines, and at one point, projectile vomit the 3 tablespoons of plain rice that Matt made for me. He is incredibly supportive, holding my hair, flushing the toilet, and surprisingly not being squeamish because anything related to bodily fluids makes him squeamish. I sit on the patio step with the throw wrapped around me. I feel normal in temperature but my body and joints hurt so much, especially my lower back. It’s a terrible pain that I’ve never felt before. I’m tired and listless and lay on the couch all day.
Later, my ulcer is still acting up. I ask Matt to pick up matzoh ball soup from Steve’s Deli. Something about that liquid gold chicken broth and giant bouncy, tender matzoh ball heals me. I am able to finally eat and hold it all in and this little act classifies as a win for Matt. I fall back asleep on the couch for three hours. I am down for the count and have never felt like this before.
March 3
I’m still feeling ill and have to cancel our dumpling classes. Fortunately, we’re able to move the majority of people to March 10 and refund a few.
March 4
I start to feel better and the rest of the day is spent on the couch resting. To know me is to know I’m never not doing something. Instead idling on the couch is my new normal and I’m mentally working at accepting this.
March 8
My friend James texts me about the coronavirus. Is it real? I tell him we don’t know enough about it and to treat it like the flu. He tells me he is sick, “like I’ve never felt before.” He’s had a cold every year but gets past it. This time, this “cold” is accompanied with a sinus infection. Even through his text, I can “hear” the uneasiness in his voice and I don’t have any words of comfort because we just don’t know enough about it. We’re not “looking” for it in the ER. Everyone is still being worked up for the flu as it’s not uncommon to see it go through April. I text him pictures of Motrin/Tylenol with instructions to alternate between the two every 4-6 hours. Take vitamins, stay hydrated, and eat well (no junk!).
‘Adapt and overcome’
March 10
It’s official: There are two confirmed cases of COVID-19 in Michigan. OK, now it’s real.
I still host my dumpling classes. Extra awareness is given to hand hygiene and food handling. There are no talks of COVID-19 and I’m relieved. We just don’t know enough about it. Really, I don’t know enough about it even though I’m a nurse.

March 11
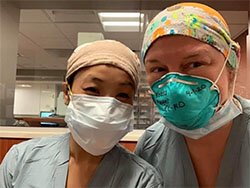
I go to work and it looks like the start of a normal ER mid-shift. To patients and their families it’s chaos, but to us nothing we can’t control. I take my assignment but today they’re distributing N95 masks with brown paper bags and we’re instructed to wear them and after exiting a patient’s room place them in the bag labeled with our names. It looks like my school lunch bag next to my workstation and my coworkers start joking about how the hospital is handing out free lunch today.
But all I can think about is in nursing school I would’ve failed if we reused our N95 masks. It was designed as a particulate-filtering facepiece respirator to filter out 95% of airborne particulates. What I’m seeing are registration clerks entering patient rooms with N95 masks without ever being trained how to properly don and doff a mask. And then worse, they dispose of them in the trash. I think our registration clerks should be protected — I think everyone should be protected, but I have this sick feeling that we’re going to lose precious equipment.
My patients are half typical ER patients: abdominal pain for X-amount of days, migraines for a 1 year or more, general weakness, and then the COVID-19 concern presenting with fever, cough, and shortness of breath. Two hours into my shift, my ANM (Assistant Nurse Manager) tells me we’re converting Area C’s wing into “COVID-19 patients” because it was designed for epidemics like this where the air is filtered to the outside of the hospital and not through the rest of the hospital.
To turn “C” into a COVID-19 zone means to now keep our double ingress and egress doors permanently closed unless badged in/out by staff. All patient rooms with sliding doors are to remain closed and we have to limit how often we enter rooms. All patients traveling to exams like CT scans, ultrasounds, or X-rays must wear a mask. We are such troopers that as ER nurses, we “adapt and overcome.” We don’t like change but understand it’s part of the controlled chaos. I haven’t even processed how I feel about working in “COVID-19 Corner.” I am now more exposed and at increased risk of contracting this virus and so I don my N95 and make sure to wash my hands and use hand sanitizer in between each room.
My mom texts me and tells me she’s worried about my safety and I reply: “I’ll be fine and it’s not like I can take a new assignment in a different area. We’re all in this together.”
Week of March 16
I’m seeing things on the news that I’ve never seen before. I’m learning more about the coronavirus as Italy, France, and Spain compete with who has the highest infection and highest death rate. It’s a competition no one wants to win but this virus is so vicious and we don’t know enough about it that people are panicking. They’re hoarding. They’re becoming violent and abandoning logic and replacing it with fear. As European countries face shortages of ventilators and supplies, so are we in the U.S. — and in our own ER. We are wearing surgical masks over our N95 masks and face shields over that. We’re wearing isolation gowns and double-gloving. Donning and doffing take 5-7 minutes each time and I’m afraid of the “hero mentality” that some of my male nurses have started to take on. Single male or married male nurses with no children volunteer to be the “COVID-19-swabber” and take nasal samples of each patient. He will put himself at risk so we don’t have to. Courageous or stupid?

We swab almost everyone that meets criteria but in my head I know we’re going to be in trouble when we run out of nasal swabs or reagents to run the results. It’s already being reported all over the news about shortage of reagents. I’m also wondering if we’re all using the same technique and swabbing all the way back into the nasopharynx where this virus lives. People already flinch and push their heads back when nasal-swabbed for the flu so I can only imagine the accuracy of trying to swab their nares in a car. I always tell patients “this is going to feel like the worse nasal tickle where you’re going to feel like you want to sneeze and pick your nose to itch it.” Done incorrectly and patients will yield negative results. I express this to my coworkers and am reassured they tell me they “aim for the brain.”
The news talks about flattening the curve so as to not exhaust the hospital’s resources but people are still coming in for non-emergent cases like pregnancy tests, STD tests, and sprained ankles on top of the emergent cases like strokes, heart attacks, COPD flare-ups, falls, and trauma. What patients complain of when they walk to the front of triage as their “chief complaint” is masked as abdominal pain and later upon assessment, they will say they feel “short of breath and have a fever.” Are they lying just to be tested? Even if they present with no temperature, do we swab them and test them? No, we cannot exhaust all our resources even though they are. I want to yell and lecture these people to STAY HOME! WASH YOUR HANDS! But through my mask I’m happy they can’t see that I’m frowning at their decision to waste our resources. The upside is our doctors are turning around patients faster and discharging them quicker to get them out of our ER. But I’m spending more time on discharge instructions to reassure them that the “right” thing to do is self-quarantine, manage any symptoms at home, and wash their damn hands singing happy birthday like they did as toddlers when they learned about handwashing.
They don’t teach you this in nursing school
Week of March 29
I haven’t been quarantining from Matt because I believe I already have safe and clean practices after each shift. We greet each other with no kisses when I enter the front door and my shoes are left outside and Lysol’d. My routine consists of immediately getting into the shower and removing my scrubs. Upon getting out of the shower and getting dressed, my mind goes through a cleansing process that tells me, “your day is over. No more ER talk.” Dirty scrubs go into the hamper to be washed in the next load.
Tonight we share an ice cream cone as we often do after my shifts — a treat for a long day’s work. We make a “plan” and what will happen if either of us gets “it.” Should we isolate ourselves from each other? No, we decide not to because we already think he’s been exposed to me. But if one of us gets “it,” does he want me to notify his parents — of course he does. Does he want to be intubated and every life-saving measure performed? Yes. Do I? Yes. My parents are in California but I would want him to notify them ASAP.
The thing about this virus is that we’ve heard how it does not care about gender, race, sexuality. It also doesn’t care if you’re in a happy relationship or not. Matt and I have been having our fair share of ups and downs pre-COVID-19 but the virus is exacerbating our problems. We get into a fight that results in five days of silent treatment. I am hurting inside because life is too precious right now and all I have is Matt. But he’s also hurting inside to give me the time of day to even hear me out. So I turn to work and pick up extra shifts floating to floors upstairs to help out where they are understaffed.
On the first floor, the ER is rapid response and we respond to all rapid response pages. We respond to all codes and intubate our own patients unlike other floors. We do it all in the ER. The new norm: hearing rapid responses constantly paged: “Anesthesia STAT with intubation to 4center room 4415. Staff with intubation to 4 Center, room 4415.” It’s not just once in a while, it’s 4, 5, 6 times during my shift. It’s surreal. But we are also now paging for Stat intubations in the EC. We have anesthesia carts outside Area C as we’ve turned these rooms into “COVID-19 CAT 1.” CAT 1 meaning “category 1 acute patients.” All other patients fall into “category 2” as they’re more stable. But because we are now dealing with extra aerosolized air, during intubation and COVID-19 is spread through droplets, it’s a risk and precaution we have to take. And now that every elective surgery is canceled, we have the anesthesia team available to do intubations for us in closed rooms.
Wanna hear something different about COVID-19 patients vs. “other” intubated patients? They are on vents longer. Rather than 4-5 days, we’re seeing 8, 9 days, sometimes longer. Longer ventilation means fewer ventilators — and fewer rooms. But why are we ventilating sooner? Because we’re watching other countries vent patients sooner to prevent ARDS (acute respiratory distress syndrome). ARDS occurs when fluid builds up in the tiny, elastic air sacs (alveoli) in your lungs. The fluid keeps your lungs from filling with enough air, which means less oxygen reaches your bloodstream. This deprives your organs of the oxygen they need to function. These patients will normally show infiltrates on their X-rays like pneumonia before turning into ARDS.
COVID-19 patients have a special pattern on their chest X-rays that other countries are finding too — “snow white patches” or “ground glass opacity” or “fluid in the spaces of the lungs.” I’m not a radiologist but I now know what to look for on these X-rays — broken glass shards just like when you have a chip in your car windshield that spreads into a larger crack. How scary is that to imagine if your lungs actually had pieces of glass shards in them? I imagine that’s what my patients feel like when they’re all coming in for the tell-tale COVID-19 symptom: shortness of breath because these “glass shards” prevent them from taking a full deep breath.
The emergency center is receiving free food from an outpouring of support from people. The amount of free pizza is overwhelming. One day we received 40 boxes of Happy’s Pizza. Another day Detroit Lion Matthew Stafford and his wife, Kelly, donated free meals from Walhburgers. The thing about all this free food is that we have to limit how much we doff and don our masks. If the virus is on the outside of the mask, we don’t want to be touching it and putting it onto our foods. Doff the masks with gloves, place in brown paper bags, throw gloves away. For those who didn’t get a break, we rush to smash a chocolate-covered Oreo that our PA’s mom dropped off attached with an individually handwritten “thank you” on them and guzzle our water bottles because we’re not staying as hydrated as we should because of these damn masks we leave on our faces all day. Then carefully don masks on again until our next sip of water, which happens hours later.
In the end, we appreciate this outpouring of love and support. But it took a pandemic for people to appreciate nurses. Pre-COVID-19, I would have the occasional patient say upon discharge, “Thank you for all that you do. Seriously, I don’t know if I could ever do your job. I don’t know how you do it.” Some days I don’t know how I do either because they don’t teach you this in nursing school.
We are not in this together
Week of April 6
My coworker posted a meme about how nurses, respiratory, techs, housekeeping, and other frontline workers are heroes. “Hero” makes me cringe because I don’t feel like a hero. A hero is courageous and virtuous. They put others before themselves. Going into war as a soldier makes that soldier a hero. They are walking in with the proper equipment and information despite following orders. My coworkers and I feel like martyrs because we’re not fully equipped with the proper PPE. Whether the appreciation continues after the crisis passes, it doesn’t matter because we have such a duty to our profession that we keep showing up. We’re all in this together.
You know who’s not in this together? Matt and I right now. Since he’s been quarantining and not working, he’s going through his own struggles. I don’t know what they are because he isn’t sharing them with me. But at the same time, I’m not asking. I am exhausted mentally, emotionally, and honestly, I’m a wreck. My sister tells me I need a good cathartic cry but when I feel like I want to cry, I can’t. I’m at work. And when I don’t want to cry, I’m at home, where I’m supposed to feel relaxed and happy to end the day … away from COVID-19, in a place that’s safe to cry. But I don’t because I think I don’t know what I’m feeling once I get home. It’s hard to come home and not be able to kiss and hug your loved one because you’re “dirty” and “contaminated.” We fight and this turns into a four-day silent treatment during which I ask him to stay in the studio next door after Matt angrily swears at me. He yells two words no one should say to anyone — ever. Especially if they love them.
April 6
I decided to pick up shifts in the ER but they didn’t have needs. Instead, they had me go to a cardiac progressive floor that’s now a partially cardiac progressive care unit and COVID-19 floor. While working up there, I learned that Kevin, my former charge nurse in the ER, passed away the night before. It wasn’t from COVID-19, but does it matter? Any death right now is too raw. It’s too much and I hide back tears because 50 is too young to leave behind two sons and a wife.
I feel foreign on this floor like when I did clinicals as a nursing student. I had to orient myself to the floor’s charting system, where the med room was, and basically get the lay of the land.
After hearing a page overhead “Anesthesia STAT with intubation to 8644 North. Anesthesia STAT with intubation to 8644 North,” I had an overwhelming sense of sadness because earlier I texted Matt to tell him that I was going to work so he could have the loft if he wanted to come in. He did not respond for four hours. I asked my landlords if they saw movement in the loft; they did not. So I asked them if they could check on Matt. Turns out, he was fine. He just didn’t want to talk to me.
He doesn’t know that what I see are patients as young as 30s to as old as 50s and 60s, people who are the same age as our parents are being intubated. Everything triggers me and the business of caring hurts me. I wish I didn’t care in this capacity right now.
April 8
I ask Matt if he wants to go for a walk to talk. We do but don’t talk about our problems, just about COVID-19 and my work. He is mostly listening and trying to be supportive and I appreciate it. But I’m torn because I want to talk about how I feel about work and COVID-19 but I also know we need to talk about our problems. We are not in this together.
Week of April 13
The ER is slowing down, seeing 60 patients rather than 120 patients. We are flattening the curve. It’s promising as the ER is finally being used for emergent cases. I haven’t seen numbers this low since I started in this ER five years ago where there would be only four patients at the beginning of a 6 a.m. shift. With that comes more redeployment to other floors where help is needed.
COVID-19 patients are intubated and the family can’t even be there. Families make decisions by phone. Making the decision to intubate even when you are next to them is scary. And it’s not a guarantee when they’re intubated that they will come out of it. It’s so scary to imagine the family making the decision and live with the guilt and fear if they make the “right” decision. I can’t imagine not being able to touch my mom and hold her hand if I were to make a decision like that. It’s purely selfish for “me” or “them” to witness and accept the decision but you know who has to live with that selfish decision? The living if the patient dies. I hate this virus and everything it’s doing to “us.”
Nurses are expected to have the same compassion for others times 100. But what they don’t tell you in nursing school is that compassion fatigue exists. What they don’t teach you in nursing school is how to identify it and deal with it.
Dorothy (Model D’s managing editor) asked me to write this column to hear what it’s like to be an ER nurse during COVID-19. I had a few ideas how I wanted to write this and as I started writing, it became a journal. In the process, I’ve been listening to Kate O’Connell’s Pandemic ER: Notes From A Nurse In Queens. Her audio letters of life in the ER in N.Y. are so chilling that I cried listening to the first four podcasts because it hits too close to home. O’Connell said something that resonated with me:
If we could recognize ourselves in others and to be kinder and gentler to one another. There is something in nursing that allows us to see the sadness and endure. It is a “gift” of nursing. We are trained to endure through that for ourselves and for our colleagues. We have to.
We are all in this together.
Wishing to test positive
Week of April 12
I am so tired this week. Fatigue, apathy. This apathy has me lying on the couch every day that I am not at work. I can’t go to work because they are low-censusing staff, which means there is more staff than there are patients. That’s OK because the rare four days in a row I have off, I’m tired and don’t care. I sleep 7-8 hours, which is unheard of for me as 5-6 is my norm. I take naps in the afternoon after I move from bed to couch. I lose my sense of smell and taste. It is a possible symptom of COVID-19 in addition to fever, cough, and shortness of breath. However, I have none of those and can’t describe what I’m feeling besides I’m just tired and nauseous, and I’m not my normal optimistic and energetic self. So I stay on the couch and peruse social media as though I care.
April 17
I return to work and find out good news: I am invited to participate in the hospital’s largest serology antibody study. I quickly register and make an appointment on my break to have my blood drawn and tested. Remember when I said I thought I had the ‘Rona? This is the time to prove it. Most of my coworkers already had their blood work drawn and when asked what their results were they are disappointed and say, “I’m negative” with the hardest eye roll that an N95 can’t hide. See, we all want to be positive because it would justify everything we’ve been going through. All the lack of PPE, donning and doffing, the emotional baggage at home and at work. The “hero” complex, the changing into scrubs before and after shift, the dry and cracked hands and peeling faces from N95 masks. We need validation that this will pass. That we are not martyrs because we have it in our blood to be caring and compassionate individuals with a cure in our blood, in our own plasma.
But no, the reality is some are testing positive by nasal swab and then testing negative by blood draw. WHY? HOW? Are these false positives? False negatives? How accurate are these tests even? I read that some test methods are only 70-80% accurate. Is that enough? Is a 30% chance of carrying COVID-19 enough to keep me inside? Or allow me to go outside? I hate this virus so much that hope seems even farther than before I even had the blood draw. I am not validated for my symptoms on March 2. For my loss of taste and smell the past few days. What is going on here?
But we are still in it together.

April 27
I got low-censused today. I knew it was coming but it doesn’t make it easier. In a department of over 250 nurses, charge nurses were taking volunteers to stay home first, then volunteers to go home early, contingents and overtime, then full-time and part-time nurses. It was my turn to stay home and not get paid or use my PTO. I have 15 hours remaining and 12 hours would leave me with 3 hours. Not enough if I’m low-censused again. I am upset. I feel personally attacked because I’m a mid-shifter getting “shafted.” They need day shift nurses to “open the ER” as they need night shift to “close the ER.” But mid-shift, we fill in gaps, we open teams and areas when triage starts to fill up. We transport and are your resource for whatever you need. We are your team players and today I’m asked to be a team player and stay home. I do because I have to and because we are all in this together.
May 6
It’s National Nurses Week, which begins each year on May 6 and ends on May 12, Florence Nightingale’s birthday. Nurses Week has even expanded to specific branches of nurses. For me, as an emergency nurse, it’s Oct. 6-12 for Emergency Nurses Week, the week that I care the most. I care about Emergency Nurses Week because it was a calculated career decision I made to become an ER nurse.
My parents, like all Asian immigrant parents, wanted their children to become doctors and lawyers. I wanted to be a lawyer until I decided in junior high and high school that I was better at math and science. I turned to science when my grandmother, my No. 1 fan, became sick and had a heart attack and then a stroke that killed her. I turned to medicine and interned 2,000 hours in the OR and ER in high school when I was deciding if I wanted to go into cardio-thoracic surgery only to turn to ER nursing because I saw that though doctors saved lives, nurses did all the work. Nurses touched and healed in a way that doctors can’t. I disappointed my parents when I chose nursing after taking the MCAT. But I made them proud when COVID-19 happened. I made them proud when they now saw on media what nurses were going through. I had my dad’s attention when he asked me to call and check in often. For Asian parents, love is expressed in subtle ways just as pride is. But for once I don’t feel like “just a nurse.”
I’ve never felt the need to designate an appreciation week for nurses much like my parents used to always say “there’s no such thing as Mother’s Day or Father’s Day. Every day is ‘Mother’s Day’ and ‘Father’s Day.’” But I think my opinion might be changing a little because damn it, we did a lot this first quarter of 2020 and head into the second quarter for a year that’s going to be considered a “wash.” We were called to do a duty we already serve not because we volunteered to but because we believe we have the capability to do it day in and day out. I used to be envious of my coworkers whose spouse would surprise their wife with a bouquet of flowers for Nurses Week. Or thank you cards with gift certificates for massages or manicures and pedicures because I never had a significant other do that for me. I realize that’s because they also think like me: “Why do you need a day to be thanked for doing your job?”
Let me tell you why. It’s because it’s a thankless job and the thanks you receive are all nonverbal. It’s the patient whose chest/back/abdominal/head pain goes away because you advocated for them in asking for pain medications. It’s the patient’s family member who tries to keep up behind you as you rush their family on the gurney upstairs to ICU where you’ve helped stabilize them and now it’s up to ICU to monitor their acute care. That family’s nod in their eyes, the slight slant in their smile that says “thank you.”
Pre-Intra-Post-COVID-19 we’re all going to see a different appreciation for nurses and I think some of it might be good, some of it might be bad. But until you walk a day in a nurse’s shoes, you don’t know and I hope you never have to find out. Leave it up to us and take no offense when I say to you, “I hope I never have to see you again. Not in this capacity.”