Inspiring pregnant women toward healthier birth outcomes
Women-Inspired Neighborhood (WIN) Network is a Henry Ford Health Detroit program that aims to improve infant mortality rates for African American families through a compassionate care model. It’s the brainchild of Dr. Kimberlydawn Wisdom, who has dedicated her career as a physician, advocate, and leader to advancing healthcare equity for vulnerable populations.
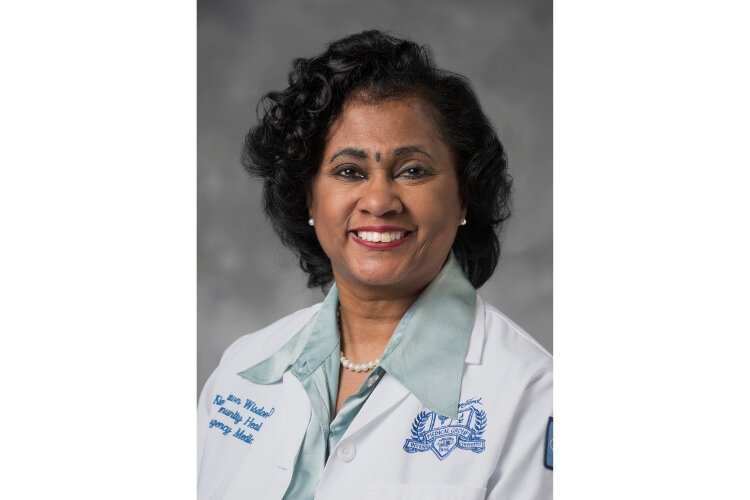
Kimberlydawn Wisdom is senior vice president of community health & equity and chief wellness & diversity officer at Henry Ford Health. She is the founder of Women-Inspired Neighborhood (WIN) Network, a program offered for pregnant women at Henry Ford Health Detroit to improve infant mortality rates for African American families.
Infant mortality rates are significantly higher in Black communities than in other demographic groups, both in Michigan and nationwide. Why?
At the individual level, a woman may not feel that she can trust the healthcare system, or that she’s being heard or respected. Many have come to providers and their symptoms have been dismissed. The sense is that there is a judgment against them, and so they may not seek prenatal care.
Then you get into the biomedical area. There’s an effect called weathering, described by Dr. Arline Geronimus at the University of Michigan as the cumulative effects of stress on women — higher cortisol levels, that sort of thing. This impacts the outcome of the pregnancy. Statistics have shown that white women without a high school diploma do better than African-American women with a degree. So, this is not just about under-resourced women. I was raised during the height of the Civil Rights movement, but even though we’re 50 years beyond where we were during that time, people of color continue to have microaggressions. Those effects and judgments take a toll.
The Women-Inspired Neighborhood (WIN) Network uses a group visit model where women learn together, get one-on-one clinical treatment from a certified nurse midwife, and mentorship from a community health worker. How does this model address those deeply entrenched social inequities?
The fix is not some rocket science, way out-there solution. We help these women feel valued. Many of them don’t have a mother, a sister, or an auntie that they can look up to, that looks after them. We link each and every one of these women with a community health worker. That person can become anything from their surrogate auntie, surrogate grandma, surrogate best friend who comes with a knowledge base they can trust. They have someone that believes in them. That goes a long way.
Our model is one where group visits — ten visits, two hours — are co-facilitated by a certified nurse midwife and a community health worker. That group visit model helps people feel like part of a sisterhood. And we have found phenomenal outcomes. We’ve had over 600 women through the program and zero preventable infant deaths.
We have a mom by the name of April, and she had three babies prior to joining WIN. She joined WIN, and she had a baby girl named Eva. When Eva was delivered, she was shocked that Eva was so big. She said, “All of my other children were born very small.” She had normalized prematurity. She didn’t know she could have a baby this healthy.
So that just shows how the community health workers — I refer to them as the secret sauce — guide these women through addressing their social needs. Addressing if they’re in a violent situation, addressing housing instability, navigating them into nursing programs or higher education, so that they feel valued, cared for, and truly loved. We don’t use the L-word very often in healthcare settings, but in many instances that’s what it comes down to.
What effect did the pandemic have on WIN Network programming and infant mortality rates in Detroit?
With social isolation and the psychological trauma people experienced based on loss, we’re pretty confident that it’s had a deleterious impact. People were frightened to come in for visits, so they wouldn’t get prenatal care, so things couldn’t be picked up as early.
We had to suspend our group visits because of COVID restrictions, so we connected with women where we could virtually. We dropped off food at their residence and did our best to get them scales, blood pressure cuffs, and dopplers. But that’s the people that we were able to actually touch. Many others were too fearful to interface with the healthcare system until time of delivery.
The beauty is that we are coming back in terms of offering robust WIN Network programming. We learned a lot of lessons from the pandemic about how to pivot quickly, how to engage women and keep them engaged, and that we need to have things like dedicated space. We’ve already started incorporating those lessons. We’re bringing back some of the things we had before, like WIN Network-labeled apparel and reunions every six months, where we take pictures and tell stories, so these women feel like they’re part of a very special club.
What does the future hold for WIN — and for infant mortality rates?
We’re in the midst of expanding to other places within Henry Ford Health. We’re going to expand to Corewell Health West, and we have already expanded to Cleveland. We’re demonstrating a model here in southeast Michigan, and then hopefully replicating that across the country. We’ve demonstrated that you can impact the infant mortality rate pretty significantly. If we’re able to spread in scale, which we’re in the process of doing, we hope to see a significant and sustained decline in our infant mortality rates.
This entry is part of our Nonprofit Journal Project, an initiative inviting nonprofit leaders across Metro Detroit to contribute their thoughts via journal entries on how COVID-19, a heightened awareness of racial injustice and inequality, issues of climate change, and more are affecting their work–and how they are responding. This series is made possible with the generous support of our partners, the Michigan Nonprofit Association and Co.act Detroit.